
A Roadmap from
The Collaborative on Housing for Health

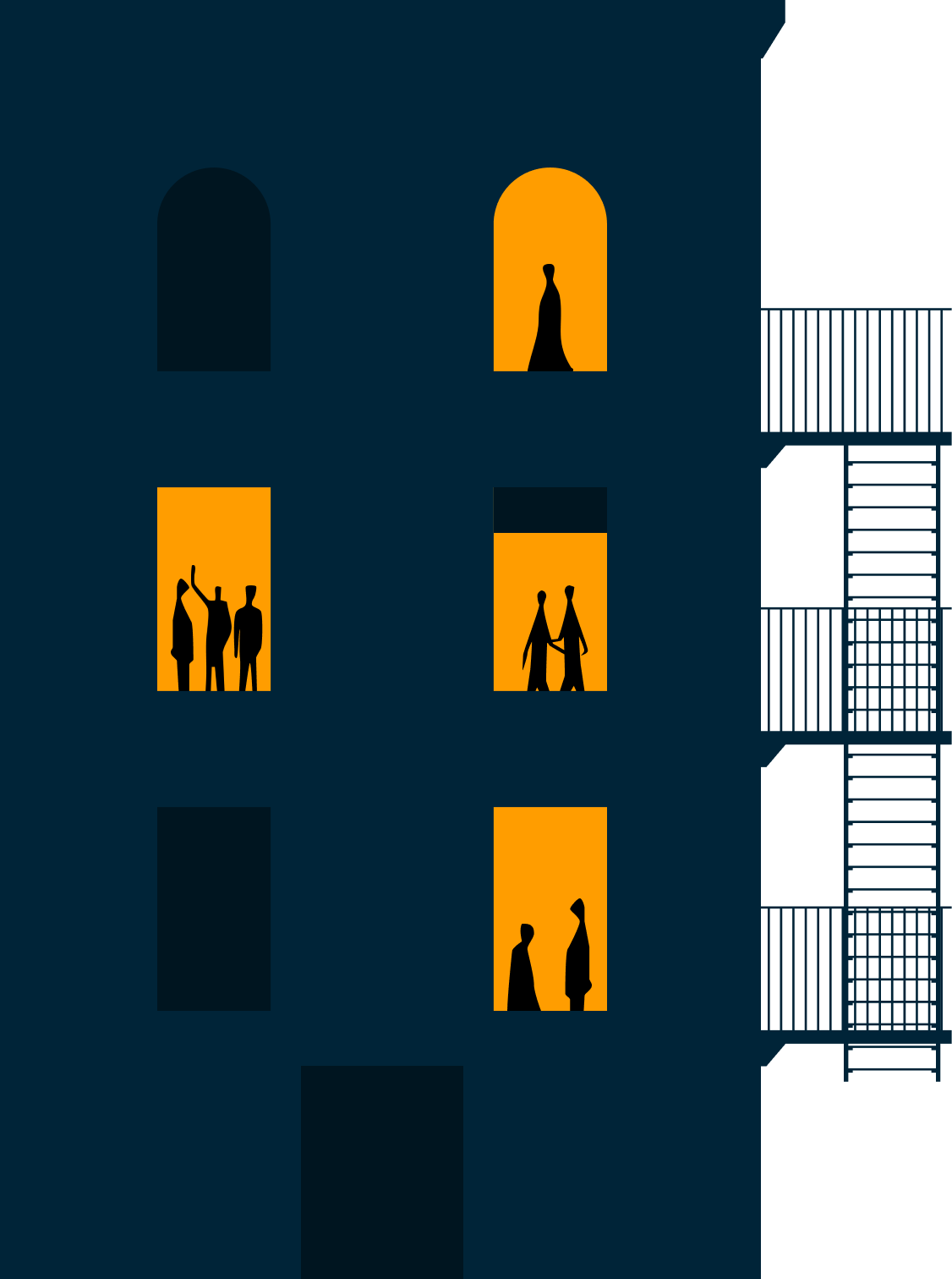
The health needs of adults experiencing homelessness have fundamentally changed in recent decades. Today's population is more likely to experience complex and co-occurring behavioral health conditions - including personality, substance use, and mood disorders, as well as serious mental illness - that our system wasn’t designed to address.
When behavioral health issues are not well managed, isolated problems spark vicious cycles – as individuals bounce between streets, shelters, hospitals, and jails. These cycles exacerbate health problems and make it more difficult to get on a path to stable housing.

EMERGENCY
EMERGENCY
RIKERS

we call this problem
high-acuity homelessness
Today, a system of seasoned providers operates dozens of effective health and housing programs, supported by billions of dollars from the City and State budgets. And yet every day, individuals fall through the cracks.
There has never been a better time to do this work.




Many stakeholders are already building momentum to address high-acuity homelessness. The shifting landscape at the federal, state, and city levels is creating the need to act. And the cost of inaction is highly visible, creating pressure on elected representatives to act.





Many stakeholders are already building momentum to address high-acuity homelessness. Shifting priorities from leaders at the federal, state, and city levels is creating opportunity. And the cost of inaction is highly visible, creating pressure on elected representatives to act.
We have the expertise, programs, and resources.
What we need are pathways that carry people across the gaps.







Building coordinated, accountable service pathways to housing and health stability for homeless New Yorkers with the greatest needs
Through data analysis and extensive input, the Collaborative developed a comprehensive roadmap to end high-acuity homelessness in NYC.
The roadmap outlines a clear vision for closing system gaps and recommends concrete steps that can be implemented with existing resources over the next two to three years to achieve lasting system transformation.
Address the most complex behavioral health cases to dramatically improve outcomes across the board
Over recent decades, homelessness among single adults has become more complex, with rising rates of personality and mood disorders, substance use, and overlapping health challenges. When these conditions are not well managed, individuals often cycle through repeated crises – bouncing between hospitals, jails, shelters, and streets.
Our analysis of administrative data shows that each year, a small but highly visible group of New Yorkers is trapped in this cycle, leading to elevated emergency healthcare usage, shelter incidents, and involvement in the justice system. These “high-acuity” New Yorkers are a small slice of NYC’s homeless: ~1% of adults experiencing homelessness, by some measures. But failure to address their behavioral health needs puts a disproportionately large strain on the system, including higher service costs, stress on provider staff and peers in shelter and other service settings, and negative impacts on quality of life for all New Yorkers. Serving high-acuity New Yorkers more effectively improves outcomes across the board.
~1,000
New Yorkers are caught in a cycle of acuity between both shelters and hospitals
~104,000
single adults spent at
least one night in shelter over a 24-month period
~6,000
experienced high-acuity in hospitals
~4,000
experienced high-acuity in shelters
In partnership with the Collaborative on Housing for Health, the NYC Department of Social Services’ Office of Research & Policy Innovation (ORPI) conducted a novel analysis using datasets from City shelters and hospitals. It found that roughly 1,000 New Yorkers were caught in a cycle of acuity between DSS shelters and hospitals – about 1% of NYC’s single adult homeless population.
Within this small group, it also found multiple distinct segments with very different needs. One segment, for example, has a “classic” supportive housing profile, with severe psychotic diagnoses like schizophrenia. Another, newer segment experiences personality and mood disorders rooted in severe childhood trauma. First line services for individuals in one segment could be wholly ineffective for another. Defining subgroups based on service needs is essential — and when we do, everyone benefits: individuals, providers, neighbors, and the City’s budget.
“It was so frustrating and exhausting to go from the hospital to the streets or from the hospital to a traumatic shelter because I would always end up right back in the hospital…I was always feeling so nervous because I knew my life was at stake, whether I was going to kill myself or someone else was going to kill me.”
– Lived expert focus
group participant

Provide practical, shared tools for staff at common discovery points to identify high-acuity individuals
As they cycle through streets, shelters, hospitals, and jails, high-acuity individuals interact with caring staff that could connect them to help. But staff in one system have little visibility into the bigger picture – and without shared data or tools, the best opportunities to intervene are often lost.
The first step is equipping frontline staff with practical tools and training to recognize when someone is stuck in a high-acuity cycle. Right now, New York has no common way to identify these individuals across systems, which leaves staff at hospitals, jails, shelters, and on the streets working in the dark.
The result: missed chances to connect people to the right services — especially during critical moments like hospital discharge, jail release, or when someone turns down services.
Analysis by the NYC Department of Social Services’ Office of Research & Policy Innovation (ORPI) found that high-acuity groups interact much more frequently with hospitals, jails, shelters, and street outreach teams than the general population of single adults served by the shelter system.
High-acuity groups interact frequently with shelters, hospitals, jails, and street outreach
“Rather than seen as vulnerable, we are seen as a threat [by doctors and hospital staff].”
– Lived expert, speaking about hospital care and hospital discharge

Empower specialized providers to deliver coordinated, accountable service pathways suited to individuals' needs
Moving from behavioral health crisis to health and housing stability is not a simple, linear process. It requires specialized expertise, coordination, clear accountability, and flexibility. But today, housing and health services are delivered by a fragmented community of providers operating a confusing landscape of programs, which challenges our ability to effectively coordinate services and match individuals to the most appropriate providers.
High-acuity individuals need specialized care to address more complex behavioral health issues
High-acuity New Yorkers need specialized services for complex behavioral health needs. Analysis by the NYC Department of Social Services’ Office of Research & Policy Innovation (OPRPI) found that high-acuity groups experience serious mental illness, substance use disorders, and personality and conduct disorders much more frequently than the general population of single adults served by the shelter system. Addressing these conditions requires expertise and training that is not the norm for most homeless services and supportive housing providers.
To address this, we need services to be embedded in coordinated pathways, not one-off programs, and delivered by specialized providers with clear accountability for achieving housing and health stability. We must empower specialized providers to develop service pathways - from identification through supportive housing - for high-acuity subgroups, working with small networks of peer organizations to share data, coordinate in real time, and track outcomes together — ensuring the right client lands with the right team at the right time. These providers must have experience, expertise, and interest in engaging high-acuity individuals, offer relevant housing and health services, and demonstrate an ability to work with partners (like SUD treatment programs). In exchange, they’ll be accountable for delivering results.
What is a “service pathway”?
A continuum of existing housing, care coordination, and clinical services offered in coordination by capable providers, that address the unique needs of high-acuity New Yorkers to move them from common discovery points to housing and health stabilty
Intensive case management
Low barrier transitional housing
Specialized transitional housing
Permanent supportive housing
“I was never made aware that there was any relationship nor communication between hospital staff and any of my support networks [like my ACT team]…. [After discharge, I never saw] any type of follow-up amongst each other or with me.”
– Lived expert

Improve system flow to connect people with the support they need when they need it
Even when housing and health services exist, high-acuity New Yorkers can’t always access them quickly enough, or at all. Critical bottlenecks — from long waitlists to complex eligibility barriers — keep people stuck in crisis instead of moving toward stability. Unblocking these chokepoints helps programs work the way they’re meant to and maximizes the impact of current resources.
In housing and health, time is as important as space. For example, a transitional housing unit might serve one person in a year — or a dozen — depending on the length of stay. That means system capacity can grow two ways: by adding more units, and by improving “flow” between them.
Fixing bottlenecks requires dynamic modeling to quantify the impact of different policy and funding decisions on system flow. With better data, advocates and decision-makers can see not just where the choke points are, but also the impact of expanding capacity or changing regulations to make the system more efficient.
Service pathways are the key to unlock this approach. They provide a shared methodology to estimate supply and demand for services using existing data, to produce actionable regulatory and funding insights that reflect ongoing changes in supply and demand.
“I was essentially my own caseworker…. I traveled around the city. I made phone calls and sent emails trying to be as proactive as possible while constantly being on the edge of a crisis. I was beyond desperate…I felt like I was dying.”
– Lived expert, describing experience on a waitlist for services
Our goal
Ending high-acuity homelessness is within our reach, but the next few years will be crucial. Our next mayor must set the vision and provide strong leadership, in close collaboration with State officials. The Collaborative is prepared to help.
In the weeks following the election, we will share additional recommendations for the next mayor and his transition team.
Over the next 2-3 years, we will make strategic investments, focusing where we are uniquely suited to advance priorities that individual service providers and government officials cannot achieve unilaterally, including:
Together we can create a cohesive, coordinated system that puts vulnerable New Yorkers on a path to health and housing stability.
Full
Roadmap
Coming
Soon
Together, we can transform fragmented services into a coordinated system that delivers real results for New York's most vulnerable residents.

The Collaborative on Housing for Health (CH4H) brings together senior government leaders, nonprofit health and housing providers, and philanthropic partners to transform how we serve New Yorkers with the most complex needs. Our goal: Create coordinated, accountable service pathways that put high-acuity New Yorkers on a path to health and housing stability.



